Amanda Sammann Launches The Better Lab to Drive Innovation in Healthcare Delivery
Amanda Sammann, M.D., M.P.H., a UCSF trauma surgeon based at Zuckerberg San Francisco General, recently launched The Better Lab, an innovative research program based on human-centered design in healthcare. With her co-founders, Design Director Susan Dix Lyons and Researcher Lara Chehab, The Better Lab is focused on addressing health care challenges through greater empathy and better design using rigorous public health methodologies.
A recent blogpost on the site by Susan Dix Lyons, How The Better Lab Got Started, traces Dr. Sammann's journey from a Stanford graduate working in finance to the trauma surgeon of today and tells the story about how she became inspired to rethink the current paradigms in the healthcare system that are discouraging to patient and clinician alike.
“THE SYSTEM WAS HORRIBLY BROKEN – AND I WANTED TO BE A PART OF FIXING IT.”
Dr. Amanda Sammann presenting at the 2016 CMS Quality Conference
She was on the trading floor when the first plane hit the first tower on 9/11. Then, the second tower was hit. Amanda Sammann was a new grad with a human biology degree from Stanford working a job in high yield bonds in New York City.That day altered the path of her life.
“I remember walking by medical tents, seeing smoke rising, people covered with ashes, and thinking that I just wanted to be down there helping,” said Sammann, a trauma surgeon at Zuckerberg San Francisco General Hospital and Founder and Executive Director of The Better Lab, a venture that uses design to study and fix healthcare challenges.
Sammann had attended Stanford during the first dot-com boom, but was always drawn to medicine. She volunteered at Stanford Hospital and worked on a novel adolescent health website – but it was the late ‘90’s and HMO’s were taking over. “It just seemed like such a horrible time to go into medicine,” said Sammann.
But the attacks on the World Trade Center in 2001 stirred something in Sammann that brought her back to her earlier passion. She loved healthcare, and she needed to be a part of it.
“I realized that if I was going to go into medicine, I would not go quietly,” she said. “The system was horribly broken – and I wanted to be a part of fixing it.”
Each step along the way of that journey ended up contributing to Sammann’s vision and creation of The Better Lab and her commitment to being a force for positive change in health.
She began by getting her Master’s in Public Health from Columbia. “Medicine is focused on fixing each individual while public health focuses on the greater good for the whole,” Sammann explained. “I wanted to have that training as well as I entered medicine in a way that I hoped would be disruptive.”
While at Columbia, she focused on informatics and technology in large-scale health interventions. It was an exciting time to be in public health, post-9/11 and during the anthrax scare, when letters containing anthrax spores were mailed to five news media offices and two U.S. Senators, killing five people and infecting 17 others. “I realized we didn’t have good systems for surveillance and monitoring of wide-spread disease,” Sammann said. She finished her pre-med requirements, and went on to UCSF to earn her medical degree.
“I showed up the first day and said I wanted to be a surgeon, where do I start?”
“I NEEDED TO GO TO A PLACE LIKE THAT.”
But Sammann wasn’t satisfied with that role as it existed.
Medical School is four years long. A lot of medical school training is undifferentiated until the end, Sammann said, which didn’t work for her. So she designed a series of electives to train medical students in surgical skills and studied the outcomes. She then created a system for students to assist with transplant donor runs to be an extra hand for the surgeons. She honed the idea of what she wanted, which included studying the process as well as the interventions so that others could learn and the work could be validated.
After medical school, surgical training takes 5 years, with 2 years of research at UCSF. Sammann wanted to use those 2 years to learn how to be innovative; to go from evolutionary change to revolutionary change. In order to do that, she felt she would have to leave the ivory tower of academia. Sammann remembers reading The Art of Innovation by IDEO’s Tom Kelley in the VA when she was on night call. Kelley, partner and co-founder of IDEO with his brother David Kelley, had built what many consider the greatest design and development company in the world – and an icon of disruptive innovation.
“I decided I needed to go to a place like that,” said Sammann.
And so she did. Sammann served as Medical Fellow and Medical Director at IDEO from 2011 to 2013, where she was immersed in the process of design thinking.
“IT WAS THE BEST PROFESSIONAL EXPERIENCE OF MY LIFE.”
At IDEO, Sammann developed the creative confidence she needed to rethink how to approach healthcare, learning in a well-established and rigorous way the path to innovation. She had the opportunity to work with mentors such as Stacey Chang, now the Executive Director of the Design Institute for Health at UT’s Dell Medical School, and to see healthcare from a “360 degrees lens.” And she did human factors research, learning how to go about asking questions.
“The first time I interviewed a patient I went in like a bull in a china shop,” Sammann said, “asking questions like a surgeon: ‘Tell me this. Tell me that.’ Then I learned you get such richer information by actually just having a conversation with the patient: ‘Oh, what game is that you’re playing? Tell me about it.’”
“If you ask pointed questions, you’re not going to get to the unmet needs,” she added. “You’re going to confirm or reject your hypotheses – not get to the real issues.”
What Sammann also discovered was that every part of healthcare – from the CDC to academic institutions to private hospitals and device companies – all wanted to do that right thing. They all wanted to find ways to innovate and improve the system. But there was “a great chasm between the companies and institutions developing the devices and services and the people providing and receiving care.”
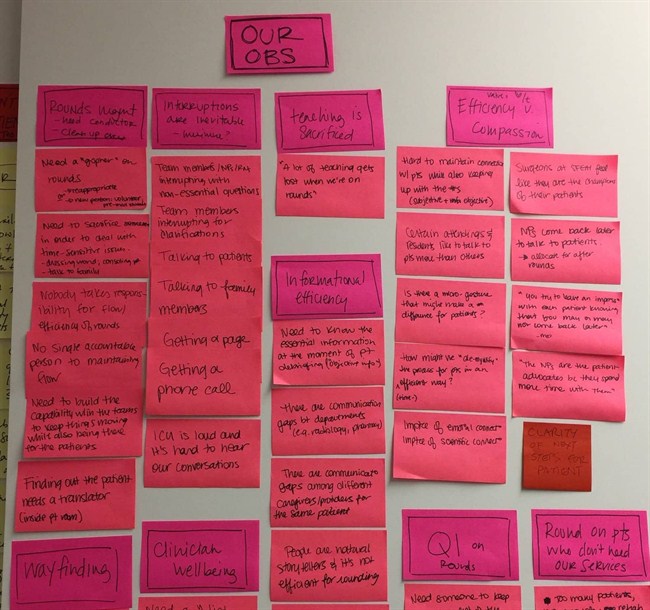
That’s when Sammann decided she wanted to start an in-house design firm at ZSFGH where the process could be studied and iterated on to implement innovations – and to do it in an open-source way where information was shared. To make healthcare better in a collaborative way.
The Better Lab was born.
“'BETTER’ IS GOOD ENOUGH FOR NOW.”
Healthcare providers, Sammann believes, need to be a part of what the tech and device companies and architectural firms are building in health care to bridge the chasm that exists – and make things better.
Sammann says that “better” is important because without it our healthcare system is unsustainable. Without it, we can’t afford to provide the care we need.
“There’s so much waste,” she says. “We can do amazing things if we can improve the system. We need to be better.”
What exactly is “better”? “Better is good enough for now under these circumstances and in this context for this patient to provide quality, efficient care, with the knowledge that everything is going to change and that we constantly need to reassess and revise and adjust to new contexts and circumstances,” Sammann says.
The big challenge is creating a culture where you’re constantly iterating within a system that can’t shut down and reboot – to create a way of constant iteration without compromising a system that needs to be excellent 365 days of the year, 24 hours a day. Sammann says you do that by starting with low-risk, low-cost incremental changes, biting off small pieces that are manageable. “Don’t try to overhaul the whole thing at once,” she says.
You also need buy-in from everyone participating or affected, finding ways to co-design solutions that come from users at every level.
“WE NEED TO BUILD A BETTER SYSTEM TOGETHER.”
Success means showing that human-centered design can work in healthcare to uncover opportunities and lead to innovative solutions. It also means marrying the design work with rigorous evaluation methods in order to study and publish research in a way that promotes wider learning in the field. And, it means figuring out a way to implement change swiftly and meaningfully in a dynamic system that can’t stop.
Sammann also wants to demystify healthcare by sharing the rich, human stories involved. To soften the boundaries of what is a very intimidating place where people go when they’re scared and confused – and to tell the stories of patients in a way that connects people to one another and deepens understanding.
“We need to break down the barriers between those who provide care, those who receive care, and those who support care,” says Sammann. “We need to build a better system together. All of us. Because we’re all part of it.”
This blogpost orginally appeared on The Better Lab website and was reproduced here in its entiretly with permission.